Treating “Bradycardia” with a Beta Blocker – A Case of Non-perfusing Rhythm
Patient Z is a 78 year old male with a medical history of ischemic cardiomyopathy who had an implantable cardioverter-defibrillator (ICD) placed earlier in the beginning of 2016 [dual-chamber, rate-modulated (DDDR) pacemaker] , hypertension and hypothyroidism. Patient Z presented to the ER after 1 episode of dizziness, elevated blood pressure to 170 systolic and bradycardia of 40bpm. Symptoms resolved en route to the ER but elevated blood pressure and bradycardia persisted. His ICD [with lower rate limit set at 60bpm] was interrogated about five months ago.
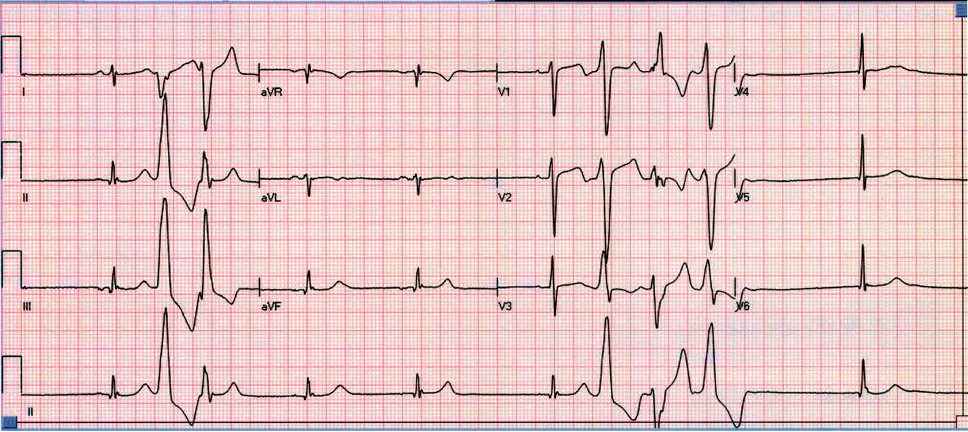
Initial work for acute coronary artery disease and other structural heart disease were unremarkable. Beta blocker was initially held given persistent pulse rate of 40s [manually and determined by portal vital monitoring system] and was placed on telemetry monitoring. Telemetry monitoring was consistent with heart rate of 60-70bpm while manually, heart rate was remarkably slow to 40pbm.
The difference between telemetry readings and manually checked heart rate is due to frequent non-perfusing Premature Ventricular Contractions that were not captured by blood pressure cuff. Given frequent PVCs, metoprolol 25mg daily was started to suppress PVCs with plans to increase it as tolerated.
There is no clear evidence that PVC suppression with beta blockers improves overall survival in patients who have no symptoms and have not had a major arrhythmic event. The only indications for the use of beta blockers for PVC suppression are for symptomatic patients or for patients with cardiomyopathy/other structural heart disease.
For patients with symptomatic PVCs refractory to beta blockers or calcium channel blockers, additional therapeutic options include antiarrhythmic medication and radiofrequency catheter ablation.